Covid-19 vaccines: what does 95% efficacy mean?
So far the FDA has approved vaccinations produced by Johnson & Johnson, Pfizer and Moderna, but what do their respective trial results tell us?


The vaccination effort has been a key priority of President Joe Biden’s first few months in the Oval Office and on Wednesday he announced that the United States is on the brink of administering 250 million doses of vaccines.
So far three covid-19 vaccines have been approved for emergency use in the US by the Food and Drug Administration, each with its own characteristics. One of the most talked about differences between the three vaccines is their efficacy, but ranking them may not be as easy as it appears.
What is the difference between covid-19 vaccine efficacy and effectiveness?
Although they are commonly used interchangeably, in the context of vaccines there is a subtle difference between ‘efficacy’ and ‘effectiveness’. Talk of a vaccine’s efficacy is related to how well it performed during clinical trials and other forms of testing, and is used to give an initial guide for how well the pharmaceutical will work.
Effectiveness is used to describe how well a vaccine works in the real world, when the results reflect a much larger group of recipients. Because the vaccines are all relatively new we are only just beginning to see how they have performed in real-world situations, but initial research suggests that they are proving very effective.
New data shows Pfizer & Moderna vaccines are 90% effective in “real-world” conditions, one key obstacle to vaccine herd immunity—
— Eric Feigl-Ding (@DrEricDing) March 31, 2021
➡️A key group with highest resistance: “Republican men”.
Also vaccine passports? We already have that for schools! #COVID19pic.twitter.com/hY8KsBceBO
How important is vaccine efficacy?
Of the three vaccines approved so far, one appears to be far less efficacious than the others. Both the mRNA-based Pfizer and Moderna vaccinations were given an efficacy of between 94–95% in trials, while the Johnson & Johnson single-dose shot is 66% efficacious. However there is some confusion about what these figures mean.
Scientific journal The Lancet has published a paper on common misunderstandings about the coronavirus vaccines entitled 'What does 95% COVID-19 vaccine efficacy really mean?' They explain the definition of efficacy by comparing the likelihood of two groups becoming infected with covid-19; one which had had the vaccine and one which had not.
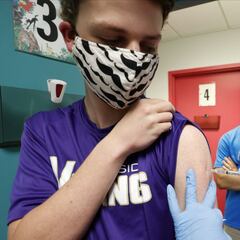
Good news: Adolescents 12 and up can now get the Pfizer COVID-19 vaccine. Hear more from Dr. Walensky about how the COVID-19 vaccine protects kids and their families: pic.twitter.com/PkRMxpBbBc
— President Biden (@POTUS) May 12, 2021
Related stories
If both groups were kept in similar conditions for a controlled period of time then the vaccinated group should have a far lower rate of infection. For example, if after three months 1% of the non-vaccinated group had caught covid-19, then scientists would expect around 0.05% of the vaccinated group to have become infected.
The study makes clear that a 95% efficacy “does not mean that 95% of people are protected from disease with the vaccine.” There are also factors unrelated to efficacy or effectiveness that could decide which vaccine is the safest option in different situations. In isolated rural communities where distribution is difficult, the one-dose Johnson & Johnson vaccination may be the best way to protect to population swiftly.